All things pelvic organ prolapse.
Your guide to prolapse. Raising the profile of this super common condition. Your most frequently asked questions answered.
As specialist pelvic floor physiotherapists (also known as pelvic health physiotherapists) we work with people experiencing prolapse all the time. We know that people want to understand their condition and have lots of questions. For example:
What is a prolapse?
Does a prolapse get better?
Why does my vagina feel heavy? What is that bulge?
Can I exercise with a prolapse?
Will sex make a prolapse worse?
There are no stupid questions. We will have heard your question before! So let's get started….
What is a prolapse?
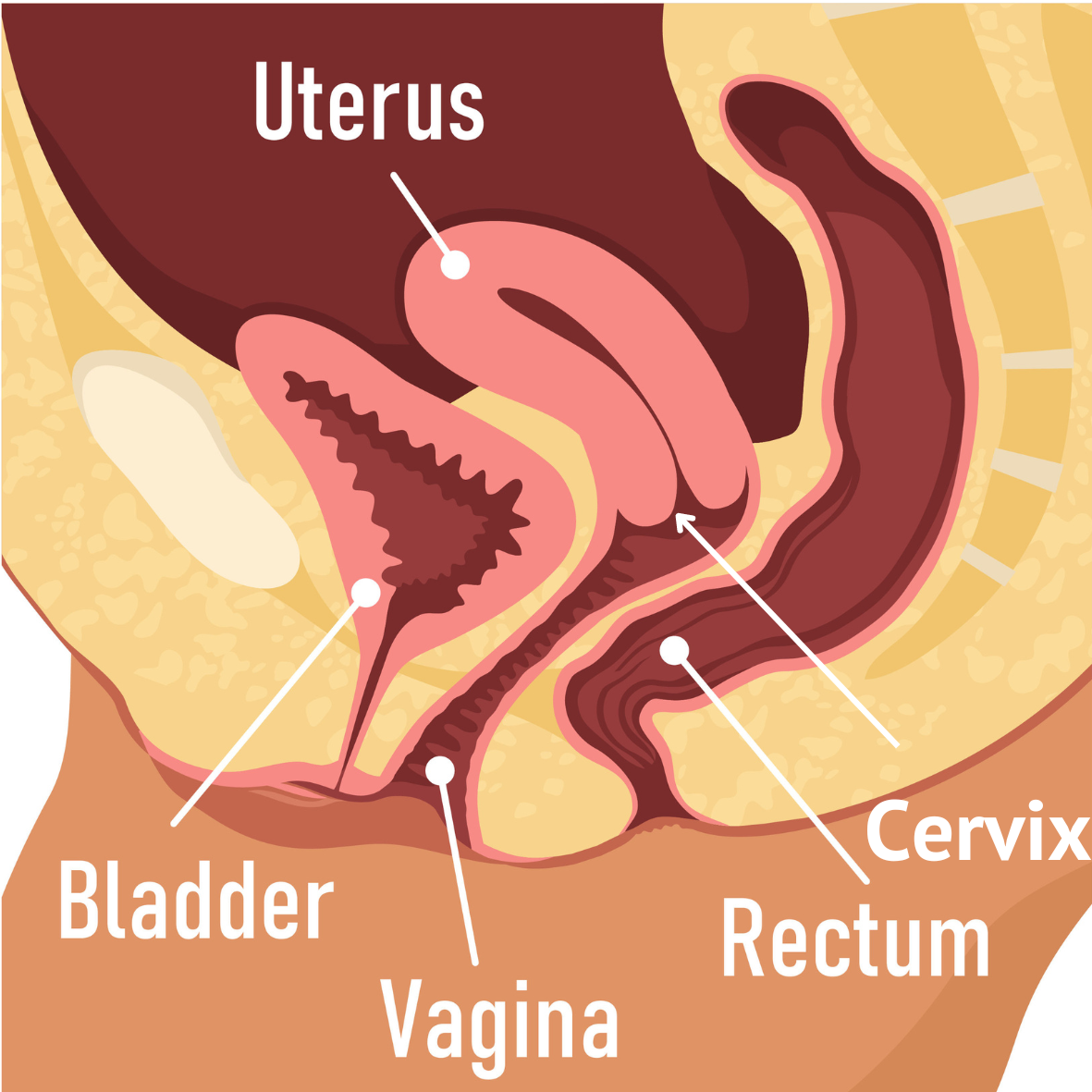
Pelvic organ prolapse is usually called ‘prolapse’. It means that one or more of the pelvic organs (bladder/bowel/uterus) moves downwards into the vagina. The different types of prolapse are given different names.
Normal Pelvic Anatomy
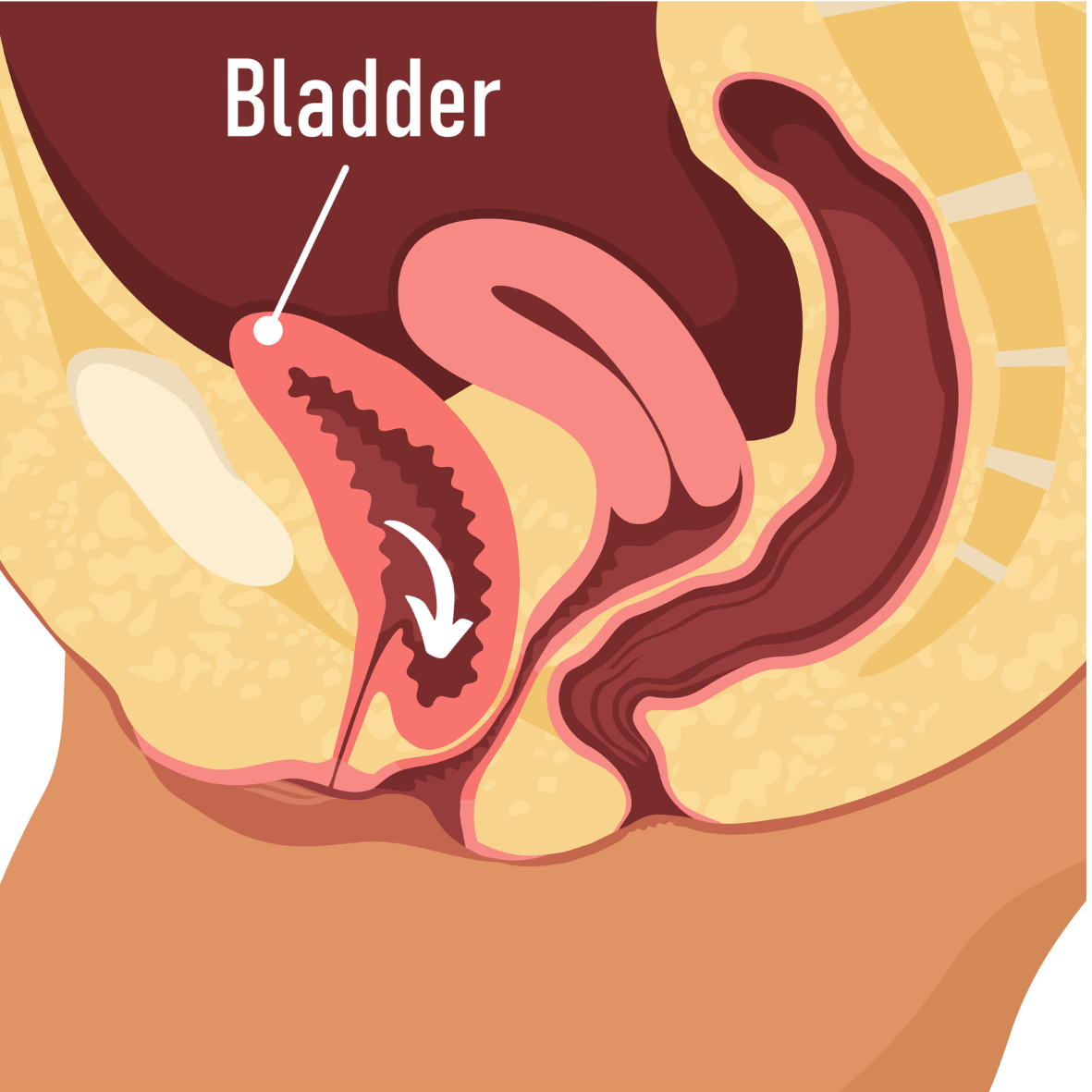
Front Wall/Bladder Prolapse
If the bladder is pushing into the vagina we call it a front wall or bladder prolapse (previously known as a cystocele).
Back Wall Prolapse
If the rectum is pushing into the vagina, it is known as a back wall prolapse (previously known as a rectocele).
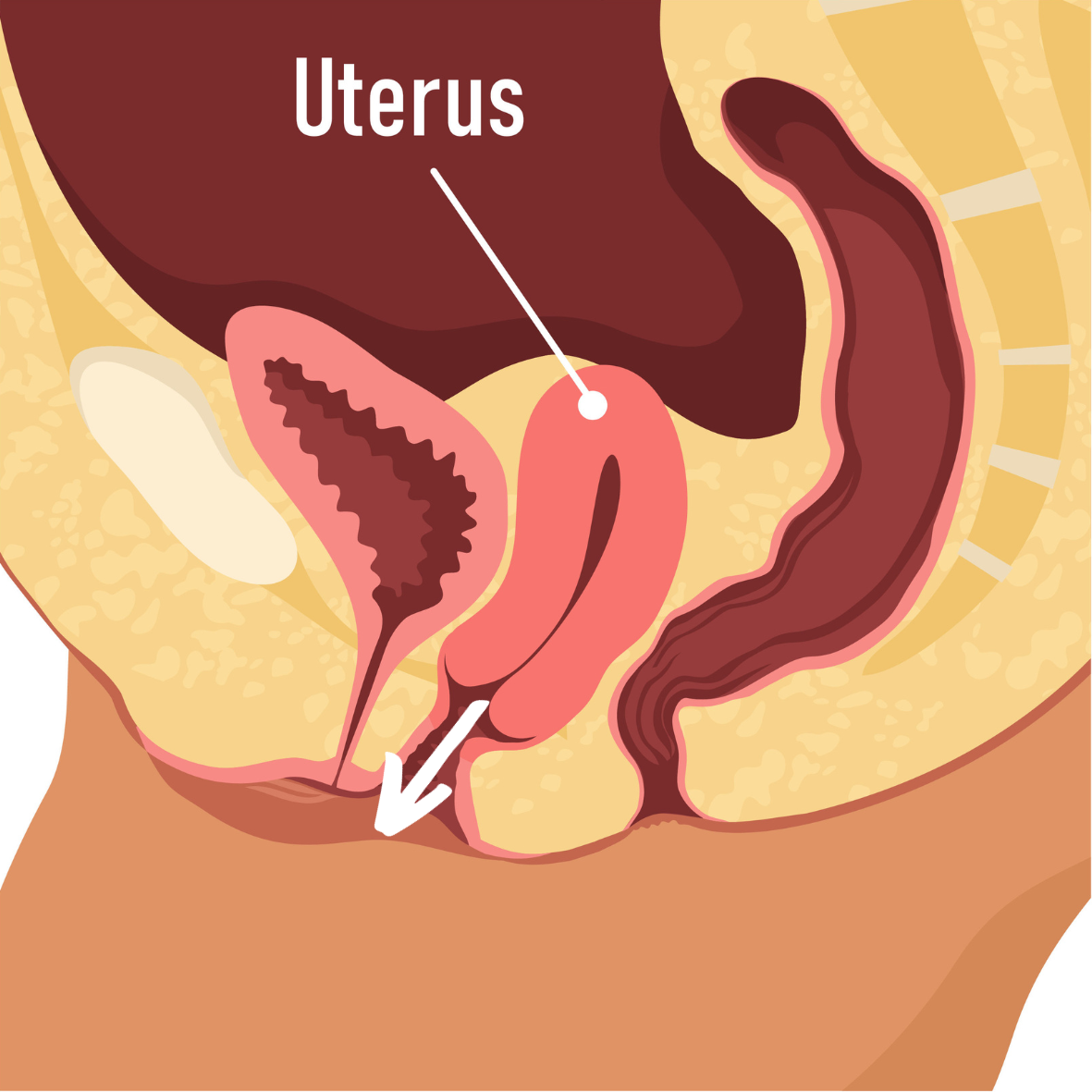
Uterine Prolapse
This happens when the uterus (womb) descends into the vagina. This will result in the cervix sitting lower in the vagina. It can involve front and back wall prolapses also.
Vault prolapse
After a hysterectomy (removal of the uterus) the top of the vagina can move downwards. The bladder and bowel can also be involved.
What causes a prolapse?
A prolapse happens when the tissue supporting the vagina becomes thinner and weaker leading to the downwards movement of organs. This can happen for many reasons, these are called risk factors. Some causes we can change and potentially improve symptoms, others we can’t.
Things we can’t change (Non-modifiable risk factors)
Getting older
Vaginal childbirth
Previous hysterectomy
Pregnancy
Use of forceps (although we can make future birth preferences)
Increased birth weight >4.5kg
Prolonged second stage of labour
Familial history
Connective tissue disorders
Things we can change (Modifiable risk factors)
Increased BMI
Repetitive heavy lifting
Constipation
Menopausal symptoms
How common is prolapse?
Figures vary from 3% to 50% of the population! YOU ARE NOT ALONE.
What are the symptoms of a prolapse?
General symptoms of all types of prolapse are vaginal heaviness or dragging. Some people may have the awareness of a bulge or be able to touch or see a bulge. Sex can be difficult or uncomfortable, or you may be very anxious about it. You can even experience pain in the vagina, lower abdomen, or back, however, this is less common.
Different types of prolapse can have different symptoms.
Bladder Prolapse Symptoms
Recurrent urine infections
Constantly needing to wee
A feeling of your bladder not being empty
Leaking urine
Difficulty weeing
Back Wall Prolapse Symptoms
Urgency for a poo
Difficulty pooing
Not feeling properly empty after a poo
Having to use your fingers to poo
Leaking wind or poo
Will a prolapse get better?
There is some evidence that a very mild prolapse (a very small bulge) can improve and potentially disappear. But we aren’t exactly clear why that might be.
Prolapse can occur straight after vaginal birth. There is lots of healing in the postnatal period so this is an example of when a mild prolapse may disappear.
What treatments are available for pelvic organ prolapse?
The best treatment for prolapse depends on many factors such as severity, age, general health and patient preference. There are two main categories of treatment for a prolapse:
Conservative management (non-surgical)
Surgical management
Conservative management
Pelvic floor physiotherapists are experts in helping you manage your prolapse symptoms. We can advise, educate and teach you about the following options:
Pelvic floor exercises
Managing sore, dry or itchy vulval/vagina skin
Improving constipation
Achieving a good bowel empty
Improving sexual discomfort
Exercise modification
Lifting modification
Pessaries - these are amazing devices that sit in in the vagina and support the pelvic organs
Surgical management
It is generally advised for more significant prolapse when a person’s family is complete or if physiotherapy has not helped. The type of procedure will vary based on the type and size of your prolapse.
Treatment within the NHS is guided by NICE guidelines. NICE guidelines are based on high-quality research and consider what are the most cost-effective treatments. More information can be found in the NICE guidelines linked below.
NICE Guidelines for prolapse can be found here.
NICE Guidelines for pelvic floor dysfunction can be found here.
Can I have sex with a prolapse?
Yes, you can! Sex will not make your prolapse worse. Sometimes it can be uncomfortable so trying different positions may help. If dryness is an issue using a regular vaginal moisturiser and or a lubricant can make sex more comfortable.
Will exercise make a prolapse worse?
This is super common question. We often get asked if exercising is bad for a prolapse. There is no evidence that exercise such as swimming or walking will cause or make a prolapse worse. In fact being inactive or sedentary is associated with pelvic floor problems like prolapse. The evidence for weight lifting making prolapse worse is mixed.
Exercise is medicine! Exercise and physical activity is so important for a healthy mind and body. It is really important to exercise in order to maintain strong bones and muscles. This includes the pelvic floor muscle. Everytime you move from getting out of a chair, to running or jumping you use your pelvic floor muscle and keep it strong.
However we know from experience that sometimes exercise can make a prolapse feel worse. In this case the NICE guidelines recommend you work with a pelvic health or pelvic floor physiotherapist to find the right level of exercise for you. We are experienced in getting people back to exercise like running, crossfit, pilates, yoga, climbing or weight lifting without symptoms.
What should I do now?
If you are experiencing any of the problems described above and would like further support you can book in for a free 15-minute telephone assessment by clicking the button below.
A final note - Important advice
If you suspect you have a prolapse always seek an assessment from a healthcare professional qualified to carry out a vaginal examination. This can be done by a GP, gynaecologist, practice nurse, or pelvic health physiotherapist. Other conditions can cause prolapse symptoms so it is important to have these ruled out.